CVS Caremark, one of the three major pharmacy benefit managers (PBM) in the U.S., stopped coverage for Eli Lilly’s popular weight-loss drug Zepbound, blaming drugs like it for driving up overall plan costs.
GLP-1 products, originally developed to treat type 2 diabetes, but are now FDA-approved specifically for obesity under brand names like Wegovy and Zepbound, are “significantly contributing to overall plan costs”, CVS spokesperson Phillip Blando told FOX Business. Removing coverage of the drug will result in an estimated client savings of 10% to 15% year over year in the anti-obesity medication space for its clients who choose to cover these medications for weight loss, according to Blando.
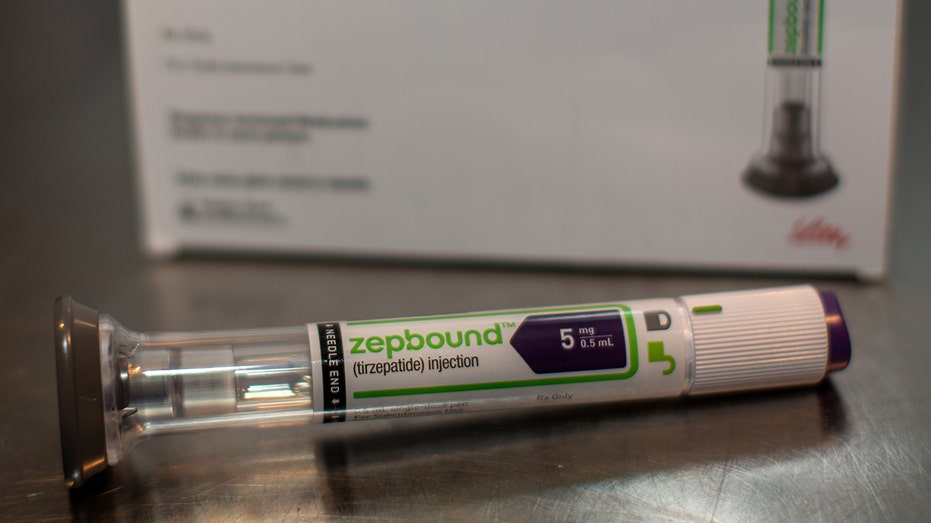
Zepbound, the brand name for Eli Lilly’s tirzepatide, was approved by the FDA in 2023 for chronic weight management in adults with obesity or overweight with weight-related medical problems. Tirzepatide was already approved to treat type 2 diabetes and was sold under the brand name Mounjaro.
TRUMP SAYS DRUG PRICES WILL BE CUT BY AS MUCH AS 90%: WHAT TO KNOW
Zepbound was widely viewed as a game-changer in the fight against obesity, after participants in a late-stage study lost up to a quarter of their body weight – making it more effective than Wegovy.
Blando said the “egregiously high list prices” for GLP-1 products that are set by drug manufacturers are “the single biggest barrier to patient access.”
“Many payers, including Medicare and numerous state benefit plans, have declined to cover GLP-1s for weight loss because of the unsustainably high prices set by brand pharma,” he said.
However, there will still be exceptions if the drug is deemed a “medical necessity.” That exemption will be reviewed “on a case-by-case basis,” according to Blando.
CVS Caremark is a subsidiary of CVS Health Corp., which also owns CVS Pharmacy. As a pharmacy benefit manager, CVS Caremark essentially acts as a negotiator between pharmacies, insurers and drug manufacturers within the prescription drug supply chain. PBMs negotiate with drug manufacturers and pharmacies to decide how much medicines cost, which drugs people can get and which pharmacies are part of their network.

Pharmaceutical giants have been critical of PBMs, saying their role needs to change. Eli Lilly previously told FOX Business that the only way to lower prices for U.S. consumers is if “intermediaries take less for themselves.”
Gastroenterologist and obesity medicine specialist Dr. Christopher McGowan told FOX Business that CVS Caremark’s decision to drop coverage of the drug is “deeply disruptive for patients who are already stable and thriving on the medication.”
RUNNING LOW ON OZEMPIC OR ANOTHER WEIGHT LOSS DRUG? A NEW TRACKER CAN HELP
“We’re now seeing insurance policy override medical judgment – forcing patients to switch to an alternative that, while still effective, has been shown in head-to-head trials to produce less weight loss than Zepbound,” McGowan said.
McGowan highlighted that GLP-1 medications “are not interchangeable in practice, even if they appear similar on paper.” He said switching medications “mid-journey can reverse hard-won progress.”
“For many, this isn’t just a simple substitution. It’s a high-stakes change that can affect long-term outcomes, trigger weight regain, or introduce new side effects,” McGowan said.
This goes beyond CVS Caremark, according to McGowan, who is concerned that its decision with Zepbound “underscores a troubling trend” in which “financial contracts between benefit managers and drug manufacturers are increasingly shaping clinical decisions.”
This means patients with fewer choices not because of what’s best for their health, but because of behind-the-scenes rebate deals, he continued.
“In obesity care, continuity matters. Once a patient finds a medication that works, preserving that success should be the priority,” he said. “Instead, we’re seeing progress disrupted and patients forced to navigate treatment changes they never asked for.”
Eli Lilly told FOX Business that the company is committed to ensuring patients have access to the treatment they need.
“While not all CVS Caremark plans are impacted, we’ve made robust efforts to proactively communicate with many of the patients who may be affected and provided clear next steps through our support programs,” Lilly said in a statement, adding that the company is encouraging patients to speak with their healthcare providers about medical necessity exceptions or alternative coverage pathways. It has also added resources on its website.
If customers do lose coverage, Eli Lilly said it expanded access through LillyDirect’s Self Pay Pharmacy Solutions, which is the company’s self-pay program, which removes some third-party supply chain entities, offering patients without coverage drugs at a discount.
The pharmaceutical giant said a patient that’s prescribed Zepbound and needs access to it without going through their health insurance can get single-dose vials for around $500.
Read the full article here










