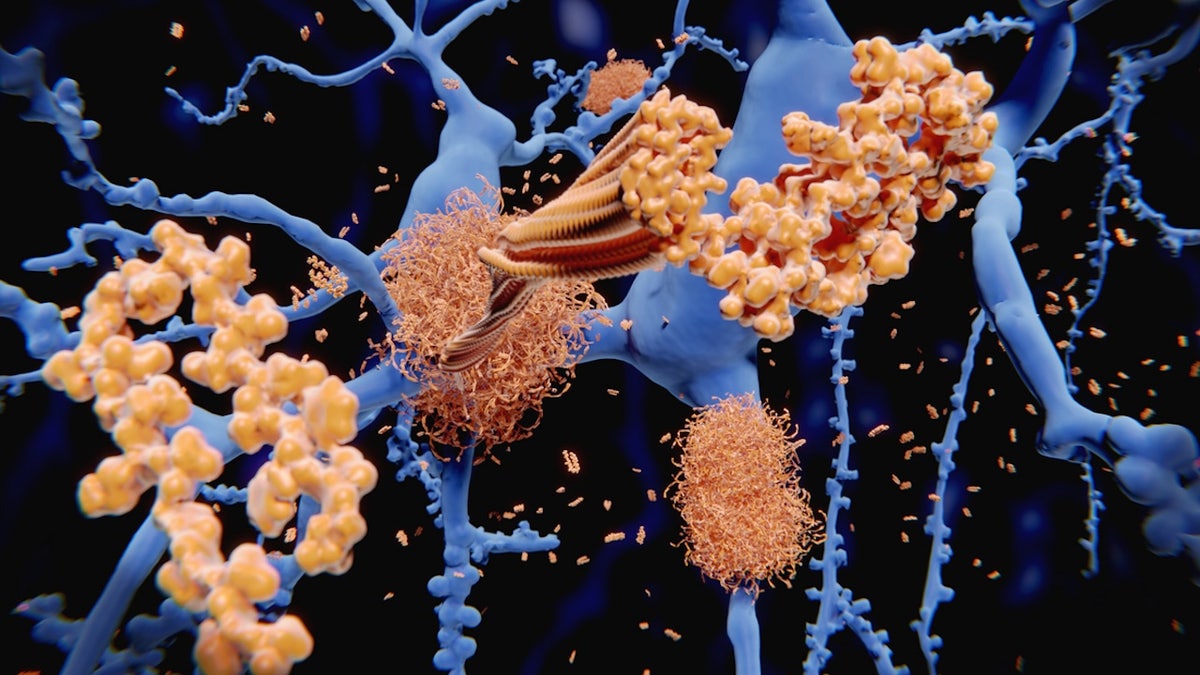
Excess fat has been linked to many health conditions, even some that impact the brain.
In the latest Alzheimer’s research, hidden fat in various parts of the body was shown to be an early warning sign of the most common dementia — as long as 20 years prior to symptoms emerging.
The study findings were presented this week at the annual Radiological Society of North America (RSNA) meeting in Chicago.
ALZHEIMER’S PATIENT, 90, SAYS SKIING AND OTHER ACTIVITIES KEEP HIM MENTALLY SHARP
“This crucial result was discovered because we investigated Alzheimer’s disease pathology as early as midlife — in the 40s and 50s — when the disease pathology is at its earliest stages, and potential modifications like weight loss and reducing visceral fat are more effective as a means of preventing or delaying the onset of the disease,” said lead study author Mahsa Dolatshahi, M.D., post-doctoral research associate at Mallinckrodt Institute of Radiology (MIR) at the Washington University School of Medicine, in a press release.
In the study, researchers assessed 80 middle-aged adults (averaging 49 years old) who did not have any cognitive impairment, according to the release.
Just over half of the people were categorized as obese. The average body mass index (BMI) was 32.31, with anything over 30 falling into the obesity category.
POOR SLEEP IN MIDDLE AGE COULD AFFECT THE BRAIN IN A SURPRISING WAY, STUDY FINDS
The researchers assessed the potential connection between signs of Alzheimer’s disease and controllable lifestyle factors, including obesity, metabolic health and BMI.
Tests included brain scans, body MRIs, cholesterol panels, and measurements of blood glucose and insulin levels.
Beyond just measuring BMI, the study used MRI technology to look closer at body fat and better determine its relationship to Alzheimer’s, the release noted.
“We investigated the association of BMI, visceral fat, subcutaneous fat, liver fat fraction, thigh fat and muscle, as well as insulin resistance and HDL (good cholesterol), with amyloid and tau deposition in Alzheimer’s disease,” said Dolatshahi.
MEDITERRANEAN DIET COULD HELP REDUCE BELLY FAT AND MUSCLE LOSS CAUSED BY AGING, STUDY FINDS
An additional finding was that higher insulin resistance and lower HDL were associated with high amyloid in the brain, which is a hallmark of Alzheimer’s.

“A key implication of our work is that managing Alzheimer’s risk in obesity will need to involve targeting the related metabolic and lipid issues that often arise with higher body fat,” said senior study author Cyrus A. Raji, M.D., Ph.D., associate professor of radiology at MIR, in the release.
In a separate study that is also being presented this week, the same research team investigated how obesity and belly fat can impair blood flow to the brain.
Three out of four Americans are overweight or obese, the researchers noted.
Meanwhile, approximately 6.9 million Americans, aged 65 and older, have been diagnosed with Alzheimer’s disease, a number that has been predicted to reach 13 million by 2050.
“The good news is these risk factors can be lowered with a healthy lifestyle and routine exercise.”
Dr. Earnest Lee Murray, a board-certified neurologist at Jackson-Madison County General Hospital in Jackson, Tennessee, was not involved in the study but commented on the results.
“We have known for some time the dangers of visceral fat on various organs of the body, likely from its facilitation of inflammatory changes — and it’s no different in the brain,” he told Fox News Digital.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
What stuck out most to Murray was how early in life the changes are noted in the brain.
“The good news is these risk factors can be lowered with a healthy lifestyle and routine exercise,” he said.

The popularity of GLP-1 medications for diabetes and obesity “will most certainly be studied” in this context as well, Murray added.
For more Health articles, visit www.foxnews.com/health
“This study also shows the importance of physicians and insurance companies focusing on prevention and the long-term benefits of modifying risk factors at an early age, as opposed to waiting for patients to develop symptoms.”
Read the full article here












